What If I Get Pregnant with an IUD? (Odds and Side Effects)

Pregnancy is always a concern when you are sexually active. Prevention is necessary until you are ready to take on the life-changing responsibility of pregnancy. IUDs are popular birth control methods due to their low failure rates and convenience of preventing pregnancy for several years with minimal effort.
However, on rare occasions, pregnancy can occur. If you find yourself wondering, “what if I get pregnant with an IUD?”, we have the details on why this could happen and what to do if you are part of that small percentage that finds themselves in this predicament.
Types Of Birth Control & Their Effectiveness
There are various birth control options for those who want to practice safe sex and prevent pregnancy. According to Planned Parenthood, condoms are 87% effective, and birth control pills are 93% effective. However, these forms of contraception can fail due to user error. Even with the best intentions, condoms can break. Birth control pills have to be administered at the same time every day to be effective. Late or missed doses can lead to pregnancy.
The patch and the vaginal ring may be convenient for those who tend to forget to take daily birth control pills. The patch is applied weekly, and the vaginal ring monthly. They prevent pregnancy 93% of the time.
The birth control shot is slightly more effective at 96% and lasts up to three months. The most effective methods of birth control are the implant and the IUD. These options last for years and the processes are reversible. Compared to their competition, these contraceptives have a 99% efficacy.
All forms of birth control have their pros and cons. Talk to your healthcare provider about the best birth control method for you. Take the time to discuss options, potential side effects, and possible issues that can arise before making any final decisions.
What Is An IUD?

An Intrauterine Device (IUD), is an effective form of birth control. The T-shaped device is implanted into the uterus. It comes in copper or hormonal form. When using a hormonal IUD, levonorgestrel (progestin) is slowly released into the body, causing it to produce a thicker cervical mucus, inhibiting sperm from reaching the egg. Hormonal IUDs may also stop ovulation. A copper IUD releases a small amount of copper causing inflammation to the uterine lining to prevent sperm from reaching an egg and implanting.
Both of these devices are inserted into the uterus by an OB-GYN and can be left in place for 3 to 10 years, depending on the type of IUD. Once removed, you can have a healthy pregnancy.
What Causes IUD Failures?
It is important to remember that no form of birth control is 100% effective. Despite their effectiveness, you can get pregnant while having an IUD. Let's discuss some rare instances that can cause an IUD to fail.
The Device Is Not Fully Effective Yet
ParaGard, the only copper IUD available, is the only IUD effective immediately. It can also be used as emergency contraception when placed in the uterus within five days of unprotected sex.
Conversely, hormonal IUDs require that IUD insertion occurs with the start of your period to be effective immediately. The Mayo Clinic recommends using back up contraception for one week to prevent pregnancy if these devices are inserted more than seven days after the beginning of your period.
Improper IUD Placement Due To Migration
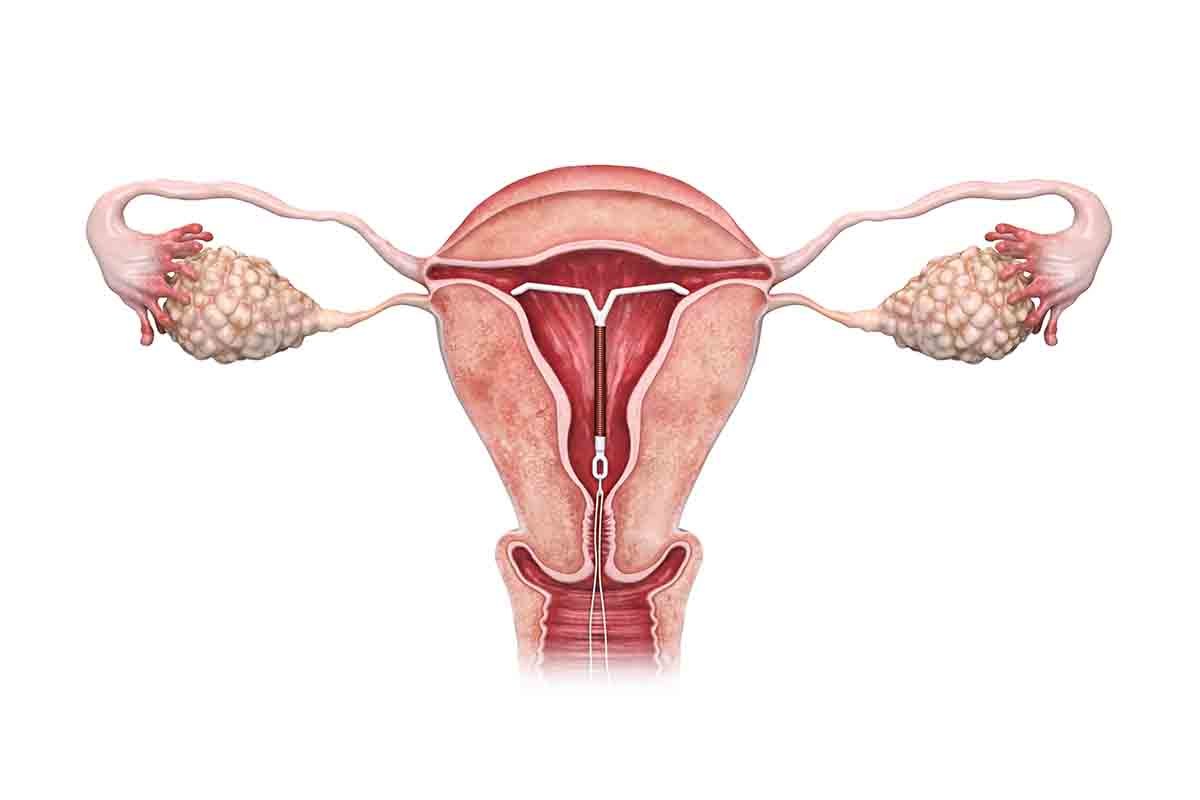
Proper placement is vital to the IUD’s effectiveness. A healthcare professional will place the device through the opening of the cervix into the uterus.
Even when an experienced provider places an IUD accurately, the device can move into the cervix or other areas of the body. This is most common within the first few months after insertion.
An IUD may migrate in people who :
- Have strong period cramps
- Have a small uterine cavity
- Have a uterus with a pronounced tilt
- Are under 20 years old
- Are breastfeeding
- Had the IUD placed immediately after giving birth
Anatomical Anomalies
Anatomical anomalies are another cause for an IUD to migrate outside of the uterus. According to the American Journal of Obstetrics & Gynecology, “retroflexed uterine positions and all uterine malformations are associated with higher incidence of malpositioned intrauterine devices.”
What this means is that if your uterus has a natural backwards tilt or if you have uterine fibroids, you are at a higher risk of expelling the device or having it move where it doesn’t belong.
Timing After Childbirth
Movement of the device can also occur if the IUD is placed in the uterus too soon after childbirth. Although you can have an IUD inserted up to 48 hours following delivery, there is a greater chance of expulsion when inserted during this time. It may be best to wait until four to six weeks after giving birth.
Watch Out For These Symptoms
Signs that migration has occurred may include:
- Missing IUD strings
- Feeling the IUD
- Your partner can feel the IUD
- Heavy vaginal bleeding
- Abnormal vaginal discharge
- Pelvic pain
- Severe cramping
These symptoms all warrant a call to your healthcare provider.
An Expired Device
Pay attention to the date that you initially had your IUD inserted. A copper IUD will remain effective for up to ten years. However, length of effectiveness can vary greatly depending on the brand of hormonal IUD that you choose.
The Mayo Clinic notes that you will have efficacy for up to 3 years for Skyla®, up to 5 years for Kyleena®, up to 6 years for Liletta®, or up to 7 years for Mirena®. Once expired, you run the risk of infection and pregnancy.
Pregnancy & Intrauterine Devices

While rare, pregnancy can occur with an IUD in about 1% or 1 out of 100 people. A positive home pregnancy test with an IUD in place may result in an extrauterine pregnancy, commonly known as an ectopic pregnancy, a life-threatening condition needing to be addressed immediately.
Symptoms of an ectopic pregnancy may include:
- Sharp waves of pain in your abdomen, pelvis, shoulder, or neck
- Severe pain on one side of your abdomen
- Vaginal spotting or bleeding
- Rectal pressure
- Dizziness
- Fainting
If you experience symptoms of an ectopic pregnancy contact your healthcare provider right away.
Your healthcare provider will conduct an ultrasound and an exam to determine if the pregnancy is viable or an ectopic pregnancy. If a viable pregnancy is confirmed, the IUD should be removed to achieve an optimal outcome for you and your baby. Not removing the IUD can result in an increased risk for infection (septic abortion or chorioamnionitis), miscarriage, abruption, and preterm birth. However, if the device has migrated to a location requiring an invasive procedure that could impact the fetus, your doctor may decide to leave the device in place.
Final Thoughts
IUDs are a highly effective contraception option for people looking for a long-term birth control solution. Low failure rates, reversability, and minimal user intervention have made IUDs a popular choice. Eventhough IUDs have a high success rate as a contraceptive method, complications can still arise.
Educating yourself on the risks and benefits of an IUD can prevent complications and accidental pregnancy. Follow your healthcare provider's instructions after insertion of an IUD and discuss any symptoms that may cause concern.

