Fundal Height Chart and Fetal Height: Measuring Your Baby

While modern ultrasounds can give us more information about our little ones than ever before, your healthcare team may perform other measurements and tests, such as fundal height measurements to estimate your baby’s length and size per week to make sure everything is progressing as expected.
To help you better understand fetal growth and how it is tracked, we’ve broken down the different tests and measurements your healthcare provider may perform and what they mean. Not all pregnancies will need all of these tests, as symphysis-fundal height measurements are sufficient for tracking the baby’s health in many low-risk pregnancies.
Related: Fetal Growth Chart (Graph Your Baby’s Progress)
What is Fundal Height?
The symphysis-fundal height (SFH) – also referred to as a fundal height – measures the distance between your pubic bone and the top of your uterus throughout pregnancy and is used to monitor your baby's growth.
The measurement of the fundus height will be tracked at prenatal checkups as the pregnancy progresses on a fundal height chart. This allows your healthcare provider to track your baby’s expected growth and fluid levels through the course of the pregnancy.
Your healthcare provider will measure fundal height at your prenatal visits. An OB-GYN may recommend additional ways to measure your baby’s growth during pregnancy as well.
When is Fundal Height Measured?
Around 24-26 weeks of pregnancy, your healthcare provider will likely begin taking a fundal height measurement at each prenatal appointment. Healthcare providers combine the fundal height with information gathered from your 20-week scan or other ultrasound tests to ensure that the baby seems to be growing appropriately.
Measuring the fundus height is not done in the first trimester or the early second trimester, because the uterus is too low in the pelvis for an accurate measurement. In early pregnancy, much of the uterus is still behind the pubic bone.
It is also uncommon for the baby’s growth to be restricted due to a health problem or condition in the first trimester or second trimester, so this measurement is not very important. Most conditions that impact the way your baby grows do not develop or start to cause problems until the second or third trimester when the fundal height measurement can more accurately be used.
How to Measure Fundal Height

Using a simple tape measure, the measurement is taken in centimeters, from the top of your symphysis pubis (pubic bone) to the top of your uterus (the fundus). Typically the number of weeks you are is about how many centimeters you should measure on the measuring tape. There is an allowance of 2 cm in either direction.
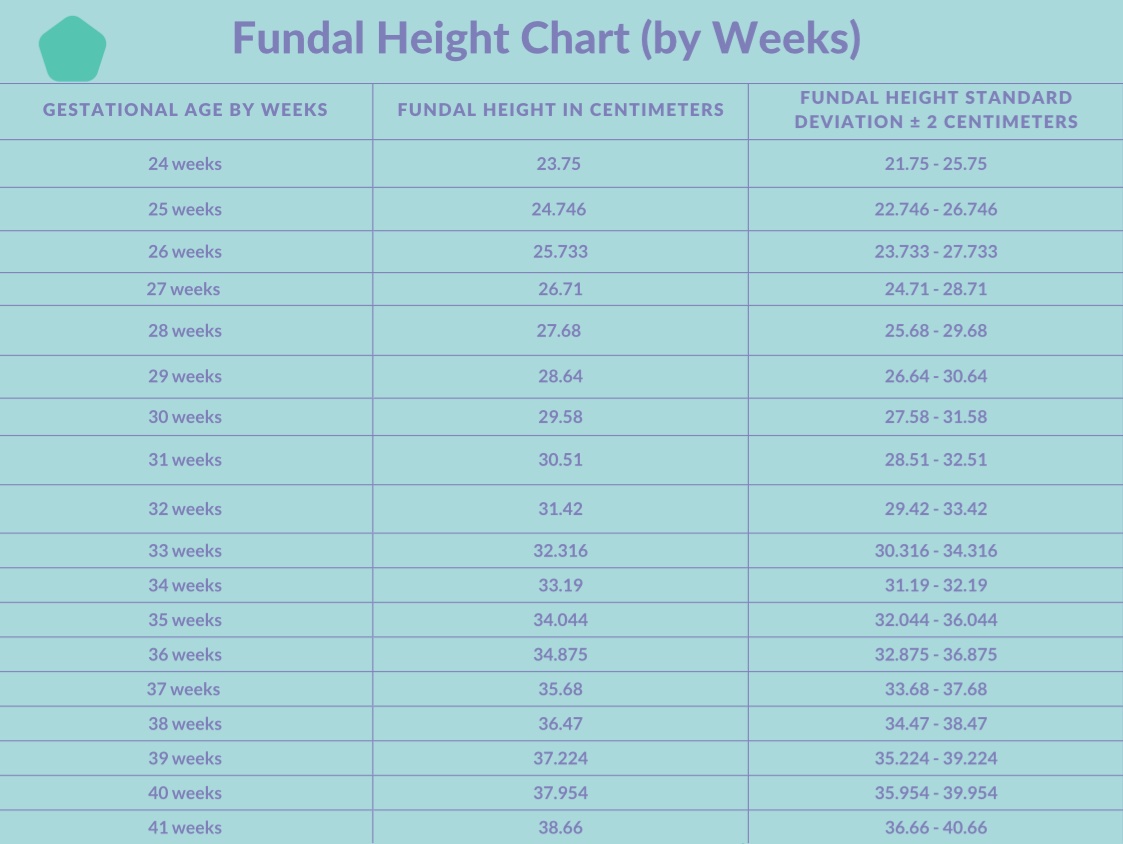
Fundal Height Chart by Weeks
Your fundal height in centimeters should align with the number of weeks along you are in pregnancy, plus or minus 2 centimeters.
For example, if you are 26 weeks pregnant, the number from the top of your pubic bone to the top of the uterus should measure between 24 and 28 cm on the tape measure.
If you are 37 weeks pregnant, your fundal height should be between 35 cm and 39 cm.
Healthcare providers can measure your fundal height from about 24 weeks until the end of pregnancy, but the measurement may become less accurate a few weeks before your due date.
Once your baby drops into the pelvis in late pregnancy, the measurement may not be as accurate and may not reflect the baby’s actual size.
What if Fundal Height is Too Low or Too High?
If there is a variation of 3 cm or more, your healthcare provider will typically arrange for an ultrasound scan to check your baby's growth and the amount of amniotic fluid. If the scan indicates a problem, the doctor will arrange for more frequent ultrasound scans to analyze and monitor growth patterns and fluid levels over time.
Fetal Growth Chart by Weeks
You can also use our fetal growth chart for a detailed look at your baby’s growth and development over time.
If there are concerns about your baby’s size and the baby is not measuring appropriately for their weeks of gestation according to an ultrasound scan, your doctor may identify this by using a fetal growth chart.
While a fundal height chart can only track the growth of your uterus during pregnancy, a fetal growth chart plots your baby’s estimated length and weight. Your doctor can then use this to look for patterns of development.
What Does Fundal Height Tell You About Your Baby?
Most people who have normal fundal height measurements can be reassured that the baby is likely growing normally and has appropriate amounts of amniotic fluid.
Even in a healthy pregnancy, there are some instances in which a symphysis-fundal height may be less accurate. If a pregnant person has obesity, is having a twin pregnancy, or has a pregnancy with more than two babies, or if there are large uterine fibroids, the most accurate way to measure and trend the growth of the baby over time is by ultrasound.
While measuring a fundus height is accurate and helpful for most people who are pregnant, ultrasounds are usually more accurate for detecting abnormal fetal growth in people who have a risk factor. For people having higher-risk pregnancies, other tests might be needed to track the baby’s growth and ensure fetal health.
You may also be scheduled for additional growth ultrasound scans if you have previously had a pregnancy with fetal growth restriction (FGR) or a large baby, as sometimes these conditions may repeat themselves in a future pregnancy.
Ultrasounds and Fetal Growth
An ultrasound scan is a procedure that uses sound waves to project images onto a computer. Ultrasounds are a fairly standard procedure during prenatal care, and most pregnant people will have at least two, one in the first trimester and one in the second trimester for the 20-week scan, also known as the fetal anomaly scan.
Ultrasounds can be performed at any gestational age during pregnancy, but the process of measuring the baby can be more complicated in late pregnancy.
The 20-week scan is a comprehensive ultrasound scan that checks for any abnormalities in growth or organ development and measures your baby. This is often when parents find out the sex of the baby.
Ultrasound Measurements
Measurements obtained during the anomaly scan or during a growth ultrasound scan include the width of the head (biparietal diameter), the circumference of the head, and the abdominal circumference.
These are plotted on a graph over a period of time. The length of the upper leg bone (femur length) may also be measured. While a baby inside the uterus cannot be weighed, when these measurements are combined together using a computer model, they can predict the size and growth pattern of the baby.
If your baby is smaller than the 10th percentile or has a small belly (abdomen), you may have more tests to assess their well-being. A measurement above the 90th percentile can be a sign of a big baby or a potential concern such as gestational diabetes and typically requires more follow-up.
Additionally, if your baby is measuring larger than average, known as fetal macrosomia, some healthcare providers may prefer or may recommend you have a cesarean delivery or induce before your due date. It is important to know that early induction or cesarean section are not standard recommendations from the American College of Obstetricians and Gynecologists for people who might be having a big baby (suspected macrosomia), and may involve more individual decision-making between you and your healthcare provider.
Additional Well-Being Tests
If your baby is not measuring their gestational age or you have other risk factors that may affect your baby’s development, your OB/GYN or midwife may order additional testing such as a non-stress test, stress test, biophysical profile testing, or a Doppler scan.
Typically these are referred to as forms of antenatal testing, which can tell your OB/GYN or midwife if your baby is experiencing more stress than expected. While these tests do not tell you the size of your baby, they can indicate if your baby is getting enough oxygen while in utero.
Non-Stress Test
A non-stress test measures your baby’s heartbeat and is called a non-stress test (NST) because it does not cause any distress to the baby.
The test usually takes 20-40 minutes, during which the technician will place a heart monitor on your abdomen to assess the baby’s heartbeat and watch the heart rate pattern over time. NSTs can be performed in the late second trimester or during the third trimester, after about 24 weeks of gestation.
Common reasons your OB/GYN or midwife may order a non-stress test:
- Diabetes
- Preeclampsia or gestational hypertension
- Your baby’s fetal weight seems low (small for gestational age, sometimes referred to as suspected fetal growth restriction, or FGR - also sometimes called intra-uterine growth restriction, or IUGR)
- Your baby is less active than normal
- There is too much amniotic fluid (polyhydramnios) or too little amniotic fluid (oligohydramnios)
- You’ve had a previous mid- or late-pregnancy loss
- You use nicotine or other substances in your pregnancy
- You are over age 35 (advanced maternal age), particularly if you have a second risk factor like hypertension or obesity
- You are past your due date
Biophysical Profile (BPP)
If, after the non-stress test, your doctor has concerns about your baby, a biophysical profile (BPP) may be done. Sometimes an NST and BPP are scheduled together ahead of time. This is usually referred to as antenatal testing.
A BPP usually combines the results of an NST reading with a scan to evaluate four factors: the volume of amniotic fluid, fetal movement, fetal muscle tone and posture, and fetal breathing. Two points are given for each part of the test, so eight points would be a favorable BPP result (plus an extra two points if you’ve already had a normal NST).
A biophysical profile may be considered or ordered if you are in the late second trimester or third trimester and have a concern such as:
- Decreased fetal movement
- Previous perinatal loss (stillbirth)
- You’re pregnant with multiples
- Small for gestational age (SGA) or suspected fetal growth restriction (FGR)
- Your baby has too much amniotic fluid (polyhydramnios) or too little amniotic fluid (oligohydramnios)
- Preeclampsia or gestational hypertension
- You suffer from a chronic or ongoing health condition such as lupus, renal disease, hypertension, or are prone to blood clots
- You are past your due date
Doppler Scan During Pregnancy
A Doppler scan is done to measure your baby’s heartbeat and the blood flow to the fetus. The sonographer watches the blood flow through the baby’s umbilical cord with a special setting on the ultrasound machine that allows for acurate tracking of
A Doppler scan may be ordered if:
- Your baby has intrauterine growth restriction.
- Your baby has oligohydramnios
- Your baby has been diagnosed with a health concern in utero
- You are having a twin pregnancy or expecting more than two babies, and there are concerns about blood flow to one or more babies
For more information on a baby’s growth and size while in the womb, consult our Fetal Growth Chart.

